No setup or maintenance fees. Pay per case. Ultrasound Experts Always Available.
Normal Ovulation, Fertilization and Early Development
.jpg/:/cr=t:0%25,l:0%25,w:100%25,h:100%25/rs=w:400,cg:true)
Normal Ovulation and Fertilization
Normal fertility is a complex process that first requires ovulation. The sperm then need to make a perilous journey to reach the ovulated egg, and the fertilized egg must travel back down the fallopian tube and implant in the endometrium, 4-7 days later. It then quickly grows into the wall of the uterus.
As soon as a single sperm enters the egg, fertilization occurs, and an even more complex process quickly occurs over the next few weeks with rapid cell division from a single cell to a fully formed fetus. By 3 weeks, the gestational sac is very recognizable by ultrasound. 4 weeks after fertilization (6 menstrual weeks) we will see the tiny developing embryo and see the first heartbeat with ultrasound. 10 weeks after fertilization (12 menstrual weeks), the fetus is mostly formed with very recognizable parts- the brain, spine, heart, face, lungs, abdomen, stomach, urinary bladder, arms, legs, hands, feet, fingers, and toes.
We are incredibly fortunate to share this miracle of life- a product of your life- with you, and see these events unfold with ultrasound.
Fertilization- truly a miracle!
Creating a new life is a truly a miracle. A spectacular miracle. Seeing that miracle and sharing it with you is a truly an honor for us.
(This is a long video with commercial breaks, but well worth watching for all of us)
Issues Affecting Fertility
Issues Affecting Fertility
Due to the complexity of normal fertilization and development, it's not surprising that a number of issues can affect fertility. These include:
- Sperm count and quality
- Cervical mucous and cervical issues
- Maternal antibodies and receptivity
- Ovarian reserve
- Ovulation
- Patency of the fallopian tube (for transportion of the sperm up the fallopian tube, and and the early fertilized pregnancy down the tube to the uterus)
- Endometrial receptivity
- Uterine malformations
- Other issues affecting the uterus or endometrium
Uterine and Endometrial Evaluation
Abnormalities affecting the uterus and endometrium
Bicornuate uterus
Septate, subseptate
Uterine didelphys
Milder forms including arcuate
click on image above for more information

Fibroids and Adenomyosis
Fibroids are common. Those closest to the cavity (endometrium) are most likely to cause bleeding.

Endometrial Issues
Polyps- commonly missed elsewhere
Intracavitary fibroids
Adhesions
Other endometrial abnormalities including hyperplasia
Ablation and post ablation
Essure coils
Ovarian Evaluation
Assessment of the ovaries

Ovarian reserve
Ovarian reserve, follicle count
Exclude premature menopause

Polycystic ovaries
Polycystic ovarian syndrome (PCOS) may cause irregular menses and contribute to infertility
Patients with PCOS also have a much higher chance of developing dermoid tumors

Other
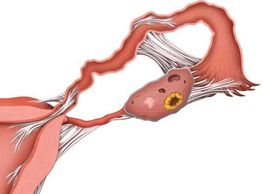
Ovarian Cysts are common- functional, hemorrhagic, endometroma, dermoid, and tumors. Also, paraovarian cysts and "pseudycysts" from adhesions.
Above is a case of ovarian cancer that could be mistaken for a "normal" cyst
Uterine Malformations
Normal
Arcuate Uterus
Arcuate Uterus
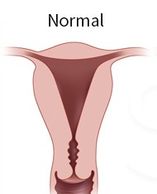
A normal uterus has a rounded top and a triangular shaped cavity with a single cervix.
The wall of the uterus is comprised of smooth muscle.
The central lining, or cavity, of the uterus is lined by a layer of cells called the endometrium.
The fallopian tubes rises from each side of the uterus near the top.
Arcuate Uterus
Arcuate Uterus
Arcuate Uterus

Arcuate uterus can be considered a very mild form of septate uterus. However, the midline 'septum' is shorter, and wider, making a U shape. In comparison, a true septate uterus shows a septum longer than it is wide, and with a V shape. Patients with arcuate uterus are sometimes, and erroneously, told they have a bicornuate uterus. Arcuate uterus has not been found to be associated with infertility or miscarriages, but there may be an increased chance of endometriosis.
Septate Uterus
Arcuate Uterus
Bicornuate Uterus
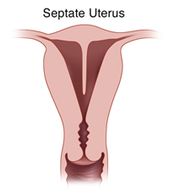
This malformation occurs when the uterine cavity is divided by a septum protruding from the fundus, but keeps the normal outer shape intact. The debate often arises on where to separate the distinction between arcuate and septate uterus. A septate uterus is a common anomaly in women with a history of miscarriages and infertility. The septum is quite variable in length, but should be at least 1.5 cm. In some cases, the septum completely divides the uterine cavity and cervix into two halves. Resection of the septum can improve fertility and reduce the risk of preterm delivery for some patients.
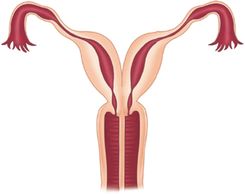
Bicornuate Uterus
Unicornuate Uterus
Bicornuate Uterus

Bicornuate uterus appears similar to septated uterus, but the outer fundus no longer has the normal rounded shape. Instead, the outer shape shows a mid indentation at least 1cm and a wide intercornual (tube) distance that can be appreciated via hysteroscopy, as well as laparoscopy. A bicornuate uterus cannot be treated with simple resection and therefore surgery is not necessarily indicated. However, there is an increased risk of recurrent pregnancy loss, cervical incompetence, and preterm delivery. Many patients are told they have a bicornuate uterus when, in fact, they may have an arcuate uterus or septated uterus.
Uterine Didelphys
Unicornuate Uterus
Unicornuate Uterus
Uterus didelphys occurs when there is complete lack of fusion, resulting in two uteruses, two cervixes, and in some cases, two vaginas. It requires special considerations when choosing birth control getting pregnant, and carrying a pregnancy to term Patietnts with uterine didelphys also have an increased chance of renal abnormalities, including an absent kidney.
Most women with uterus didelphys experience no symptoms, although some may experience dyspareunia as a result of a vaginal septum. Others have problems with vaginal bleeding. There is also an association with endometriosis.
Unicornuate Uterus
Unicornuate Uterus
Unicornuate Uterus
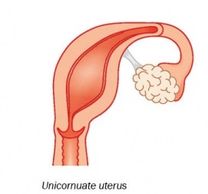
This form of uterine anomaly occurs when the uterus is predominantly formed by just one of the two paired Müllerian ducts. This abnormality has been shown to have significantly greater chance of infertility, miscarriage, and preterm delivery. On coronal 3D images, the uterine cavity no longer shows a normal triangular shape, but rather assume a banana shape. However, unicornuate uterus is typically missed with standard 2D ultrasound. In part for this reason, all fertility patients should have 3D coronal images of the uterus.
Issues of the Fallopian Tube
Normal Pregnancy
Normal Pregnancy
Normal Pregnancy

Normal pregnancy depends on a patent (open) fallopian tube for both transport of sperm up the fallopian tube near the ovary, and transport of the fertilized blastocyst down the tube toward the uterus.
Hydrosalpinx
Normal Pregnancy
Normal Pregnancy
A blocked fallopian tube can fill with fluid (hydrosalpinx), and then is predisposed to developing infection.
Hydrosalpinx
Normal Pregnancy
Endometriosis

Blockage may be caused by endometriosis, prior infection, scarring, or unknown causes
Hydrosalpinx may be confused for ovarian cysts or other conditions
Endometriosis
Inflammation, Infection
Endometriosis
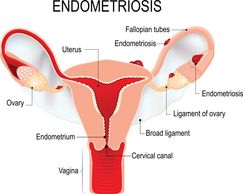
Endometriosis may produce scarring and blockage of the fallopian tubes
Inflammation, Infection
Inflammation, Infection
Inflammation, Infection
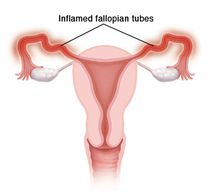
The fallopian tube may become inflamed or infected, interfering with function.
Scarring
Inflammation, Infection
Inflammation, Infection
Scarring with adhesions may block the fallopian tube. Adhesions may result from prior surgery, infection, or endometriosis.
Pelvic Pain and/ Or Abnormal Bleeding
Additional Information
For more detailed information, please see additional pages here, or visit https://YourWomensClinic.com